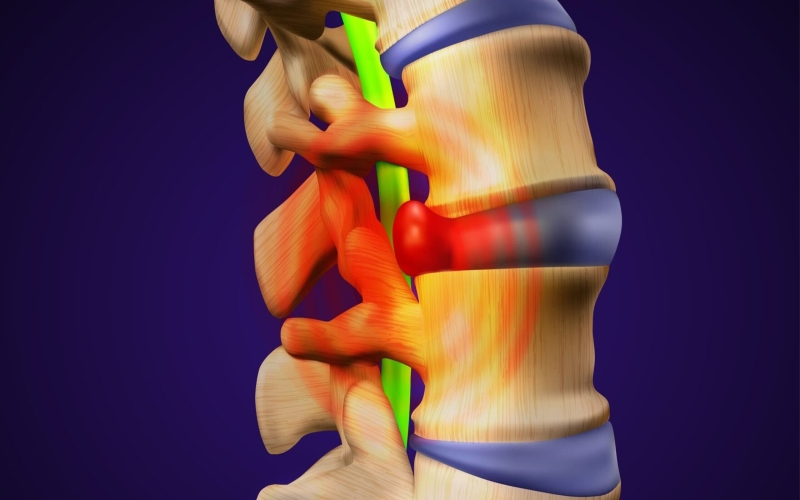
Millions of people worldwide suffer from herniated discs, which can cause pain, disability, and discomfort. Herniated discs develop when an intervertebral disc’s soft, gel-like center protrudes through its robust outer shell, pressing on adjacent nerves. This pressure can cause localized back pain, spreading pain, numbness, and arm or limb weakness. Herniated disc management requires understanding causes, symptoms, and treatment choices.
The spine’s complex vertebrae and discs provide stability, support, and flexibility. However, age-related degeneration, acute traumas, genetic predispositions, repetitive strain, and obesity can damage these discs, increasing herniation risk. Herniated discs can affect any spine area, usually in the lower back or neck. Lifestyle factors like bad posture, inappropriate lifting, and sedentary behaviors may increase disc herniation risk. Educating people about preventive measures and early intervention tactics is crucial to reducing the adverse effects of this severe condition on their health.
Herniated Disc Diagnosis
The best way to know if you have a herniated disk is to consult your doctor. They may perform a physical exam to diagnose your pain. Your doctor will examine your back for pain. They may request that you lie on your back and lift or move your legs. Your provider may also check your knee and ankle reflexes, walking ability, and ability to feel vibration, light touches, and pinpricks.
You may also undergo further tests to rule out other causes of pain or identify inflamed nerves:
X-rays: Standard X-rays can’t detect herniated disks, but they can show your doctor your spine and rule out fractures or tumors.
Myelogram: This technique measures spinal cord pressure with an X-ray and dye injected into the spinal fluid.
CT scan: This scan combines X-rays from different angles to assess your spinal cord and surrounding structures.
MRI: Radio waves, a magnetic field, and a computer create 3D images of the spinal cord and surrounding structures in an MRI. The MRI can locate the herniated disk, examine it, and identify damaged nerves.
Electromyogram: Your doctor may use these tests to check for nerve injury or compression. In the EMG test, a gadget detects muscle cells’ small electricity when nerves stimulate them. A needle electrode in a muscle captures its electrical activity to detect abnormalities.
Nerve conduction tests (NCS): In this test, an electrode at one body site stimulates nerves with small electrical impulses while other electrodes detect them at another. Your doctor can detect nerve injury by measuring electrical impulse travel time between electrodes.
Treatment options for herniated disc
Medications for herniated discs include the following:
Non-prescription pain killers: Your doctor may provide non-prescription pain medication for mild to moderate pain. Acetaminophen, ibuprofen, and naproxen sodium are options.
Neuropathic drugs: These medications disrupt nerve signals to reduce pain. Gabapentin, pregabalin, duloxetine, and venlafaxine are examples.
Opioids: Many doctors hesitate to prescribe opioids for disk herniation due to their adverse effects and addiction risk. If other medications don’t work, your doctor may prescribe opioids temporarily.
Cortisone shots: If oral medications don’t work, your doctor may suggest a corticosteroid injection. This medication can be injected around spinal nerves. The needle can be guided via spinal imaging.
Therapy
Your doctor may recommend physical therapy for pain. Physical therapists can demonstrate herniated disk pain-reduction activities.